CBT (Cognitive Behavioral Therapy) vs DBT (Dialectical Behavioral Therapy): Understanding Their Differences and Applications
CBT vs DBT: Which is best for you? Cognitive-Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) are two distinct therapeutic approaches that have proven effective for various mental health issues. While both methods aim to improve emotional regulation and coping strategies, they differ significantly in their techniques and target populations. CBT focuses on changing negative thought patterns, whereas DBT emphasizes the importance of mindfulness and acceptance in managing emotions.
Individuals dealing with conditions such as anxiety or depression may benefit greatly from CBT’s structured format, which encourages patients to identify and challenge distorted thinking. Conversely, those struggling with intense emotional swings, often typical in disorders like borderline personality disorder, may find DBT’s emphasis on emotional regulation and interpersonal skills more suitable.
Exploring the key principles and applications of both CBT and DBT can help individuals make informed choices about their mental health treatment options. Understanding these therapies reveals valuable insights into how different strategies can lead to healing and personal growth.
Foundations of Cognitive Behavioral Therapy
Cognitive Behavioral Therapy (CBT) is grounded in distinct principles that guide its practice. Understanding its historical background and core techniques is essential for appreciating its role in mental health treatment.
Key Principles of CBT
CBT operates on the premise that thoughts, feelings, and behaviors are interconnected. By modifying dysfunctional thoughts, individuals can positively influence their emotions and actions.
Key principles include:
- Cognitive Restructuring: Identifying and challenging negative thought patterns.
- Behavioral Activation: Encouraging engagement in positive activities to counteract avoidance behaviors.
- Skill Development: Teaching coping skills that enhance resilience and adaptive coping strategies.
These principles are instrumental in treating various mental health conditions, such as anxiety and depression.
Historical Context
CBT emerged in the 1960s, paralleling the rise of cognitive psychology. Its development was significantly influenced by Aaron Beck, who identified the role of distorted thinking in depression.
As a reaction against psychoanalytic approaches, CBT emphasizes a structured, goal-oriented method. The integration of cognitive and behavioral techniques provided a comprehensive framework for addressing emotional distress. This approach gained recognition for its empirical support through numerous studies demonstrating its efficacy.
Core Techniques and Applications
CBT employs various techniques tailored to individual needs. Common methods include:
- Thought Records: Tools for tracking and challenging negative thoughts.
- Exposure Therapy: Gradual exposure to feared objects or situations to diminish anxiety.
- Mindfulness Practices: Techniques that enhance present-moment awareness and reduce rumination.
These techniques find applications in treating conditions like PTSD, obsessive-compulsive disorder, and phobias. CBT is adaptable and can be delivered in individual or group settings, often with a focus on practical skills and actionable strategies.
Click here to learn more about CBT.
Essentials of Dialectical Behavioral Therapy
Dialectical Behavioral Therapy (DBT) incorporates unique principles and strategies to address emotional and behavioral challenges. Its development and skills provide a structured approach to fostering emotional regulation and interpersonal effectiveness.
Fundamental Concepts of DBT
DBT is built on several core principles, most notably the dialectical philosophy. This concept emphasizes the synthesis of opposites, such as acceptance and change. The therapy seeks to validate clients’ feelings while also encouraging them to make positive changes.
Another key principle is the focus on mindfulness, which teaches individuals to be present and fully aware of their thoughts and feelings. This awareness helps clients observe their emotional responses and reactions without judgment, fostering better emotional regulation.
DBT also employs a structured focus on the therapeutic relationship, encouraging open communication between therapists and clients. This creates a safe space for exploration and growth, essential for effective therapy.
DBT’s Evolution and Influences
DBT was developed by Dr. Marsha Linehan in the late 1980s to address complex mental health issues such as borderline personality disorder. The therapy is influenced by cognitive-behavioral techniques and mindfulness practices, integrating them into a coherent framework.
Its evolution has included adaptations for various populations, including adolescents and those struggling with substance abuse. Researchers and clinicians have expanded DBT’s application beyond personality disorders to treat mood disorders, PTSD, and eating disorders.
The therapy combines Western psychological theories with Eastern philosophy, particularly mindfulness and acceptance strategies, making it a versatile and effective form of therapy.
DBT Skills and Strategies
DBT includes four primary skill modules: Mindfulness, Distress Tolerance, Emotion Regulation, and Interpersonal Effectiveness.
- Mindfulness: Focuses on enhancing one’s ability to observe thoughts and feelings without judgment. This skill encourages awareness of the present moment.
- Distress Tolerance: Teaches strategies for managing crises without resorting to harmful behaviors. Techniques include self-soothing and improving the situation.
- Emotion Regulation: Aims to help clients identify and change unhealthy emotional responses. Skills include understanding emotions and reducing vulnerability to unpleasant emotions.
- Interpersonal Effectiveness: Offers strategies to improve communication and assertiveness. This skill empowers individuals to set boundaries while maintaining healthy relationships.
These skills are fundamental to DBT, enabling clients to manage emotions and improve their quality of life.
Click here to learn more about DBT.
Comparing CBT and DBT: CBT vs DBT
Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) are both effective treatment modalities, but they differ significantly in their approaches, goals, and applications. Understanding these distinctions can aid in selecting the appropriate therapy based on individual needs. Both therapies have been used to treat mental health disorders and substance abuse.
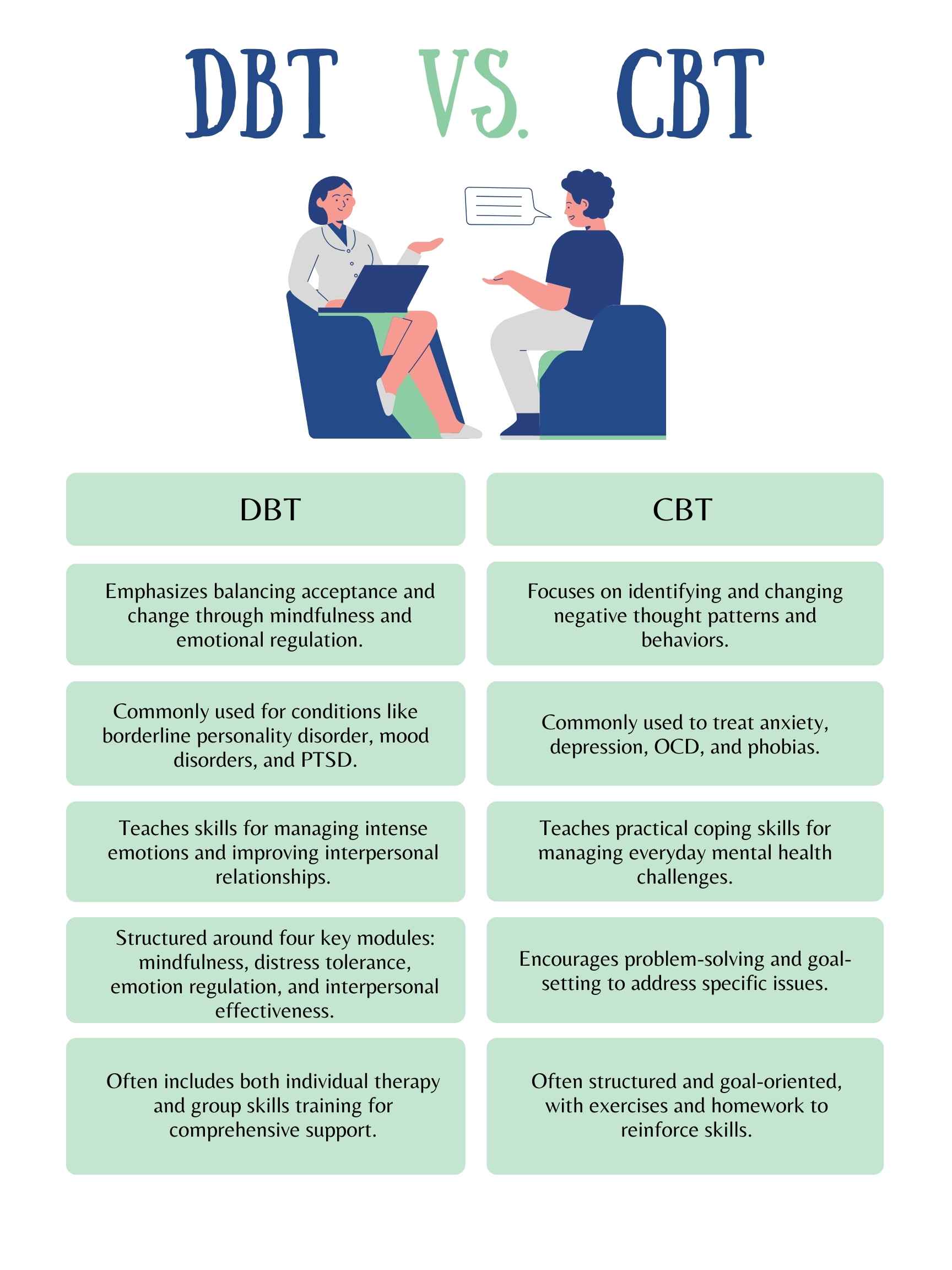
Differences in Therapeutic Approaches
CBT primarily focuses on modifying dysfunctional thoughts and behaviors. It employs a structured and goal-oriented process, emphasizing the connection between thoughts, feelings, and actions. Clients learn to identify and challenge negative thinking patterns.
In contrast, DBT integrates cognitive-behavioral techniques with mindfulness practices. It targets emotional regulation and interpersonal effectiveness. The therapy is typically delivered in both individual and group settings, promoting skills training alongside traditional therapeutic methods.
Contrasting Treatment Goals
The primary aim of CBT is to alleviate symptoms of mental health disorders by changing negative thought patterns. It is typically structured around specific problems, leading to measurable outcomes and symptom relief.
DBT, while it also addresses symptoms, focuses more on enhancing emotional and interpersonal skills. This therapy is especially beneficial for individuals with intense emotional responses and self-destructive behaviors, aiming for acceptance and change simultaneously. Goals are often broader and more focused on improving quality of life.
Both have been shown to be effective in treating addiction and substance use disorders.
Efficacy and Suitable Conditions
Research indicates that CBT is effective for a range of conditions, including depression, anxiety, and phobias. Its structured nature allows for consistent application across various mental health issues.
DBT has shown notable success in treating borderline personality disorder (BPD) and other conditions involving emotional dysregulation. Its emphasis on emotional awareness and skills training helps clients manage difficult emotions and improve relationship dynamics. The choice between CBT and DBT often depends on the individual’s specific needs and challenges.
When comparing CBT vs DBT, it is important to have an open mind. A combination of both can be helpful and is often used in certain mental health treatment programs.