There’s a kind of fear that lives in the body when your child is in crisis.
You wake up with it. You fall asleep with it—if you sleep at all. You second-guess every word you say, every silence you leave. And worst of all? You don’t recognize the version of them you’re trying to help. The anger, the withdrawal, the panic, the shutdown. It feels like you’ve lost access to your own child.
When nothing seems to be working—when therapy feels surface-level and your child can’t (or won’t) explain what’s happening inside—there is another approach. One that works with the brain, not just behavior.
It’s called EMDR therapy.
And while it might sound like “one more thing to try,” we want to show you why this might be the thing that finally meets your child where they actually are—not where people keep expecting them to be.
Learn more about our EMDR therapy services in Massachusetts.
Why Crisis Brains Don’t Always Respond to Traditional Talk Therapy
When the nervous system is overwhelmed—by trauma, fear, grief, or prolonged emotional distress—the brain shifts into survival mode.
That survival mode is incredibly adaptive in the moment. It helps your child get through danger, unpredictability, or harm. But when it stays “on” for too long, it stops being protective and starts becoming damaging.
And here’s the thing: survival-mode brains aren’t good at talking about feelings. They’re wired to react, not reflect.
So if your child is spiraling in panic, rage, or total emotional shutdown, and talk therapy doesn’t seem to help, it doesn’t necessarily mean they’re resistant or beyond reach. It might just mean their brain can’t access the part that talks right now.
EMDR therapy was built for this kind of brain. For crisis minds. For trauma responses that words can’t reach.
How EMDR Actually Works (Without the Jargon)
EMDR stands for Eye Movement Desensitization and Reprocessing.
Here’s what that really means: during EMDR, a therapist helps your child focus on a specific memory, emotion, or body sensation while using bilateral stimulation—usually side-to-side eye movements, taps, or sounds.
Why? Because this kind of stimulation activates both sides of the brain, which supports the natural way memories are processed during REM sleep.
In a brain that’s experienced trauma, memories can get stuck—almost like a looping video with no off switch. EMDR helps the brain “unstick” the memory and refile it as something that happened then, not something that’s still happening now.
It doesn’t erase the memory. It helps remove the emotional charge.
So instead of reliving it over and over, your child can remember without falling apart.
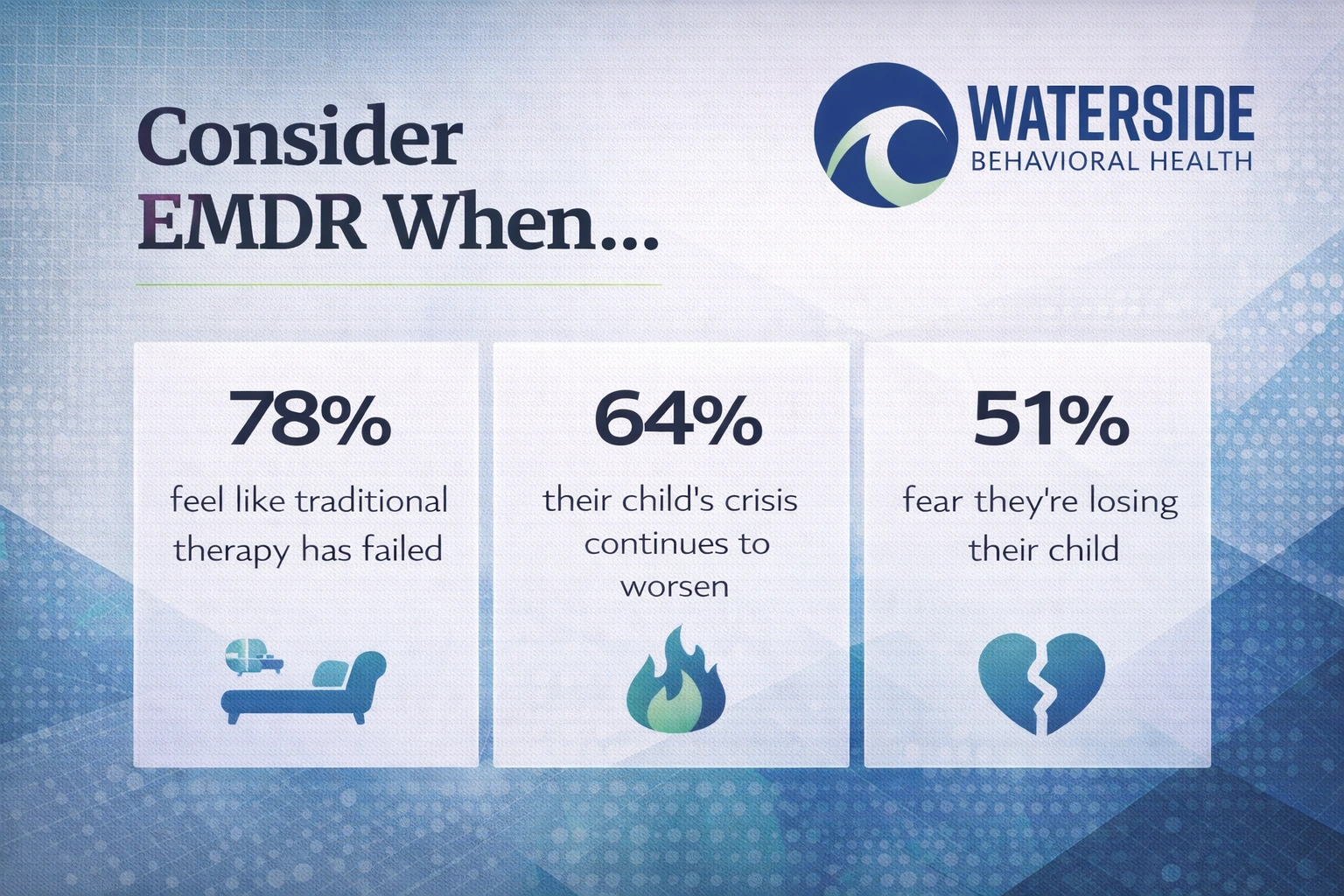
Why EMDR Helps When “Nothing Else Is Working”
You may have already tried a lot.
Weekly therapy. Psychiatric meds. Crisis hotlines. School intervention teams. Maybe even residential treatment.
And if your child still feels unreachable—or if they get worse when asked to talk about what’s happening—EMDR might be the right next step.
Here’s why:
- EMDR doesn’t require verbal processing. Your child doesn’t have to tell the whole story for their brain to begin healing.
- It works with emotional stuck points, not just behavioral symptoms. That means it targets the root, not just the reactions.
- It’s often faster than traditional therapy for trauma and anxiety—because it’s working directly with how the brain processes pain.
One mother from Plymouth County, Massachusetts told us:
“We’d tried everything. Then my daughter did EMDR. And it was like—for the first time in months—she came back to herself.”
That doesn’t mean it’s instant. But it’s often the first approach that makes a dent in the wall.
It’s Not Just for “Big T” Trauma
Sometimes parents hesitate because they think EMDR is only for major trauma—like combat or assault.
But trauma is personal.
Your child might have been affected deeply by:
- Social rejection or bullying
- Grief and sudden loss
- Medical procedures or accidents
- Chronic invalidation or pressure
- Identity-based discrimination or fear
- Witnessing violence or emotional chaos
If your child’s brain registered the experience as overwhelming or unsafe—and it hasn’t been able to move on from it—EMDR might help.
We’ve used it successfully with clients who don’t even remember the specific event, but who carry the symptoms in their body, sleep, or emotional responses.
EMDR in a Treatment Setting—What to Expect
At Waterside Behavioral Health, EMDR isn’t a one-size-fits-all quick fix. We follow a structured, trauma-informed protocol that begins with trust and safety.
The general process looks like this:
- Stabilization and preparation. Your child learns grounding skills and practices emotional regulation.
- Identifying targets. These could be memories, fears, body sensations, or patterns of distress.
- Bilateral stimulation. The therapist uses movement, tapping, or tones while your child lightly focuses on the target.
- Processing and reflection. The brain starts to shift how it stores the memory or emotion. This part is often nonverbal.
- Installation of a new belief. Once the emotional charge is reduced, your child can replace old beliefs (e.g., “I’m unsafe”) with new, adaptive truths (e.g., “I’m not in danger now”).
We never force reprocessing before someone is ready. We don’t push stories they don’t want to tell. Your child leads, and we follow with clinical skill and compassionate pacing.
What Families Often Say After EMDR
“They’re sleeping again.”
“The panic attacks are happening less.”
“They actually opened up to me, just a little.”
“They’re more present.”
“It’s not a miracle, but it feels like a beginning.”
That’s the power of nervous system-level change. It’s not always loud. But it’s deep.
And for families in Bristol County, Massachusetts, we want you to know—this kind of care is available close to home. You don’t have to wait until things are worse.
FAQs About EMDR Therapy for Teens and Young Adults
Does my child have to “believe in” EMDR for it to work?
No. Many clients come in skeptical and still benefit. EMDR doesn’t rely on belief—it relies on the brain’s natural ability to process when supported correctly.
Is EMDR scary or retraumatizing?
Not when done properly. We always begin with safety, regulation, and pacing. If your child feels overwhelmed, the session pauses. They are in control.
How quickly does EMDR work?
Some clients feel shifts in a few sessions; others take longer. It depends on the complexity of the issue and readiness to process. Healing is not rushed.
What if my child won’t talk in therapy?
EMDR can still help. Because it’s not talk-based, your child doesn’t have to explain everything. Some clients barely speak during sessions and still improve.
Is EMDR covered by insurance?
Often, yes—especially when delivered by licensed clinicians within a program or outpatient setting. We can help you explore options.
Can EMDR be used alongside other therapies?
Absolutely. It can enhance existing work with other providers or be a focused track within a broader treatment plan.
You Don’t Have to Wait for Rock Bottom
If you’ve been holding your breath for months—waiting for the breakdown, waiting for the breakthrough—we see you.
You don’t have to wait for things to get worse to explore something different. EMDR therapy is a door. Not a rescue, not a reset button—but a way forward.
Call 774-619-7750 or visit our EMDR therapy in Massachusetts to learn more. When everything else has felt like noise or dead ends, this might be the thing that quietly opens the door back to your child.