I didn’t walk into treatment with hope. Not the first time. Not even the second.
Honestly, I went because I ran out of reasons not to. Everything else had stopped working. I couldn’t fake being okay anymore. But I also couldn’t imagine sitting in a room and talking about my feelings again, like that alone would magically make life bearable.
So no—mental health treatment didn’t “save” me in the way people sometimes talk about. It didn’t pull me out of a burning building. It didn’t fix me.
But it did give me a way back.
A quiet one. A slow one. But real.
Explore mental health treatment options in Massachusetts.
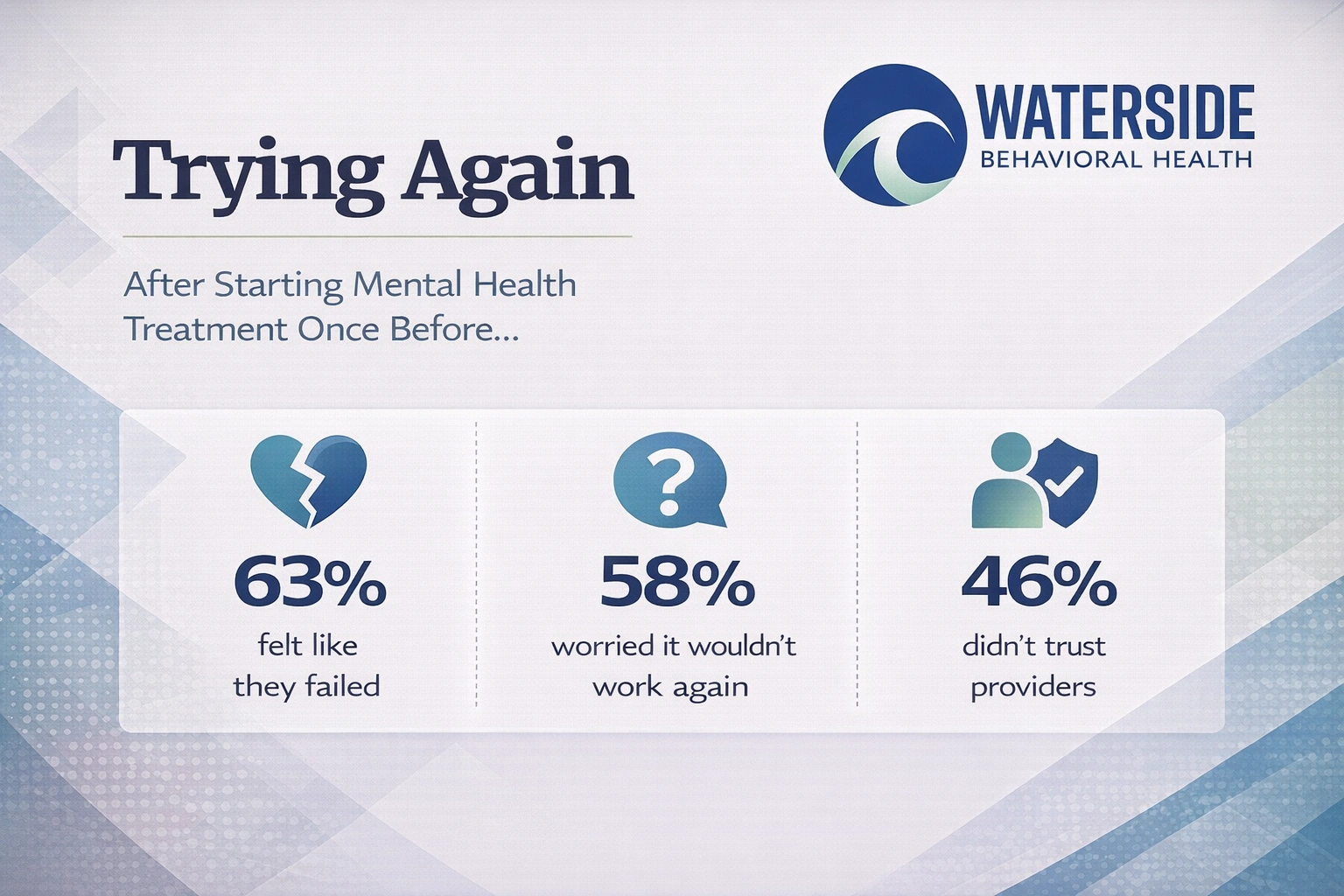
I’d Tried Before—and It Didn’t Work
If you’ve ever left a therapy session feeling like nothing changed, I know how that feels.
I’d been in treatment before. Different places, different people, same result: I walked out just as empty as I walked in. Maybe more. Because every time it didn’t work, it made me feel more broken. Like maybe I was the problem—not the process.
So when someone suggested trying again, I rolled my eyes.
But here’s what changed this time: I didn’t go in looking to be fixed. I just showed up with my truth.
That I was tired.
That I didn’t believe this would help.
That I didn’t want another worksheet or breathing exercise.
That I just wanted someone to see me and not look away.
And when that’s how I entered the room—walls up, honesty on the table—it turned out I’d made more space for healing than I realized.
I Wanted to Be Proven Wrong (Even If I Wouldn’t Admit It)
Here’s the thing I couldn’t say out loud at the time:
Part of me wanted it to work.
I didn’t trust the process, but I also didn’t want to keep living like I was. I didn’t want a miracle. I just wanted something—a small crack in the gray, a moment where I didn’t feel like I was slowly disappearing from my own life.
What I didn’t expect was that mental health treatment could make room for my doubt. No one told me to “just be positive.” No one demanded I be vulnerable on day one. I didn’t have to believe in recovery to take the first step toward it.
That was new.
The Shift Didn’t Come All at Once
There was no big breakthrough moment. No single session that cracked me open and set me free. Honestly, it was the opposite.
It was slow. Uneventful. Borderline boring sometimes.
But in that steadiness, something happened: I noticed myself noticing again.
- I noticed when my thoughts started spiraling, and I could name it instead of getting dragged under.
- I noticed when I felt something other than numb, and didn’t immediately question whether I deserved to.
- I noticed when I said “I’m okay” and realized I kind of meant it.
That’s the thing about real recovery—it rarely comes with fireworks. More often, it’s a quiet return to the parts of you that still want to be here.
I Had to Learn That Treatment Isn’t a Rescue Mission
I spent a long time thinking help had to feel heroic.
That if therapy didn’t save me, it wasn’t working. That if I still felt sad, or disconnected, or stuck, something had failed—either me or the system.
But over time, I started seeing treatment differently.
It wasn’t there to rescue me from my life. It was there to sit with me in it—and offer tools, not ultimatums.
Mental health care gave me a flashlight, not a map. And slowly, I began to see the outlines of a way forward.
I Found a Different Kind of Fit
One thing that made a huge difference? Changing the type of care.
What didn’t work for me in the past wasn’t just “treatment.” It was a mismatch—between me and the modality, me and the provider, me and the space.
This time, I found someone who didn’t rush me.
Someone who didn’t pathologize my silence or over-celebrate my wins.
Someone who didn’t mind when I showed up angry, or tired, or both.
I also found value in group therapy—something I swore I’d never do. Sitting with other people who weren’t trying to perform recovery, but just trying to survive it? That cracked something open for me.
The biggest shift, though, came from realizing I wasn’t required to like treatment in order for it to work. I just had to stay open long enough to see what could be different.
And for people in Plymouth County, Massachusetts, I want to say this: you don’t have to go far to find real, human care. You just have to find the right fit.
I Don’t Feel “Healed.” I Just Feel Present
This part’s important.
I’m not writing this from some mountaintop. I still have hard days. Still deal with intrusive thoughts. Still wake up sometimes and wonder if anything I’m doing matters.
But now… I also have a place to take that.
I have a process. A practice. A reminder that when the weight comes back, I don’t have to carry it alone.
Mental health treatment didn’t make me whole. But it did help me stop hollowing myself out.
And that matters more than I thought it would.
I Stopped Asking Treatment to Prove Itself
One day I realized: I was holding therapy to an impossible standard.
I wanted it to erase everything. To undo the years. To rebuild my sense of self and prove to me that life was worth showing up for.
But that’s not what therapy does.
It doesn’t undo. It doesn’t erase. It offers a different lens—a way to hold your story without getting crushed under its weight.
Once I stopped demanding a transformation and started accepting the process, things got clearer.
I didn’t get fixed. But I got freed.
For Anyone Who’s Tried Before and Got Burned
If you’ve left a therapist’s office feeling worse…
If you’ve been told to “just try harder”…
If you’ve felt like a failure because you didn’t get better fast enough…
Please hear this: You are not the failure. That space just wasn’t built for you.
Try again. On your terms. With new questions. With fewer expectations. With more honesty.
In Bristol County, Massachusetts, I’ve seen people come back to therapy after years of avoiding it—and find something different, because they were different.
You don’t have to fake hope. You just have to be willing to see if something better is still possible.
FAQs for People Who Feel Like Treatment Failed Them
What if I already tried therapy and it didn’t help?
Then you know more than you did before. Use that knowledge to find a better fit—different provider, different approach, different pace. You haven’t failed.
I quit halfway through. Can I start over?
Yes. You’re not disqualified. Starting again doesn’t mean starting from scratch. It means continuing from where you actually are.
What if I don’t trust therapists?
That’s okay. Trust isn’t required on day one. Good providers know how to build it slowly, without pressure.
Is it worth trying group therapy?
It can be. Hearing others say what you thought no one else felt is powerful. You’re allowed to observe first. You don’t have to perform or prove anything.
Do I have to take medication?
No. Medication is one option—not a requirement. You can explore it without committing to it. Your body, your choice.
How is Waterside different?
We listen to skepticism. We don’t push for perfect engagement. We respect where you are, and we walk with you at your pace. There are treatment options in Massachusetts that won’t make you feel like a checkbox.
This Isn’t a Pitch—It’s a Door That’s Still Open
If therapy didn’t change everything the first time… welcome to the real version.
Change doesn’t always come in bright lights or sudden shifts. Sometimes it comes in the quiet choice to try again.
Call 774-619-7750 or visit our mental health treatment in Massachusetts to learn more. You don’t have to trust it completely. You just have to be willing to not give up on yourself—yet.