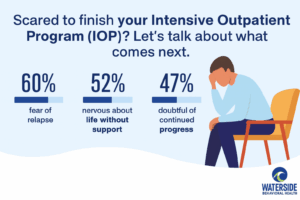
Even when everything on the outside looks fine, the idea of finishing your Intensive Outpatient Program IOP can stir up a quiet panic.
You’ve shown up. You’ve talked about things you swore you wouldn’t. You’ve maybe even started feeling things that had been buried for years. And now what?
That doesn’t mean you’ve failed. It means you’ve changed.
It means you’ve built something worth protecting.
Let’s talk about how to do that.
Explore our Intensive Outpatient Program IOP in Massachusetts
Why Ending IOP Feels Like a Free Fall
If you’re high-functioning, you’ve probably lived most of your life being the person who holds it together. That’s part of why IOP felt safer than expected. It was structured but didn’t require you to “start over.” You could do the work without dropping everything.
But now that you’re nearing the end, you might be feeling:
- Like the rug is about to get pulled out from under you
- Afraid your progress was more about the environment than your actual readiness
- Quietly panicked at the idea of navigating emotions without the daily check-in
This is not about being dramatic. It’s about being self-aware.
IOP works because it scaffolds your life. You’re not wrong to wonder what happens when the scaffolding gets pulled away.
Transition Planning Isn’t Optional—It’s the Second Half of Treatment
If you’re someone who’s always handled things privately, the idea of still needing support might feel like weakness. But let’s be honest—doing it all alone was never the goal.
The goal is sustainability. And sustainability is a team sport.
Transition planning includes:
- Identifying triggers that haven’t shown up yet (because IOP was a buffer)
- Planning for high-risk moments like travel, holidays, or job stress
- Setting up non-negotiables (therapy, community, routines) to hold your progress
At Waterside Behavioral Health, we treat transition like part of the program, not an afterthought. Because relapse isn’t the only risk—burnout, emotional isolation, and subtle drift are just as real.
You’re Not “Done”—You’re Evolving
Let’s kill the graduation fantasy: You don’t walk out of IOP into the arms of a fully healed life.
You walk out with tools. And you need somewhere to use them.
One client put it this way:
“I was terrified of ending group. Not because I wasn’t proud of myself, but because I didn’t want to go back to being the version of me that could keep a secret that big.”
– IOP Client, 2024
That version of you who learned to hide the drinking? Who could white-knuckle through a hangover and a staff meeting without blinking? That person served a purpose. But you don’t have to go back there.
Aftercare exists to help you stay visible—to yourself and others.
High-Functioning Doesn’t Mean Invincible
This is the danger: You look fine. You sound fine. People stop asking how you’re doing. And slowly, the internal slide begins.
That’s why we recommend layered support after IOP:
- Weekly therapy with someone who speaks fluent “high-functioning”
- Continued group sessions (even monthly) for a reality check
- Medication management when appropriate (for anxiety, depression, sleep, etc.)
- Boundaried check-ins with trusted people—not just casual venting
- Alumni circles or regional recovery groups where you don’t have to wear the mask
And if you’re staying in the area, our Plymouth County IOP options include built-in alumni access points—so you’re not just drifting into “after.”
You Don’t Have to Pretend You’re Not Scared
Let’s name it: You’ve probably spent a lot of energy convincing people (and maybe yourself) that you’re fine.
That same energy doesn’t serve you anymore. Recovery isn’t about proving anything. It’s about staying honest enough to know when you need a hand.
If fear is showing up, pay attention.
- Fear of “slipping” isn’t weakness; it’s self-awareness.
- Fear of being without a safety net is wisdom, not fragility.
- Fear of losing this new version of yourself is a sign that this version matters.
Use that fear. Let it guide you into the next layer of support.
What Realistic Aftercare Looks Like (Not Just a Pamphlet)
We’re not here to check a box and send you off with a list of therapists.
Here’s what aftercare might actually look like with us:
- A real schedule. Not “if you feel like it,” but every Thursday at 6PM, you’re in group.
- A recovery buddy. Someone you can text when things get loud in your head.
- Workplace boundaries. For clients who work high-stakes jobs, we help you build invisible systems—like calendar buffers, no-meeting Mondays, or end-of-day recovery anchors.
- Family strategy. Not every family is ready for your healing. We help you set up conversations (or silence) that protect your space.
This isn’t “ongoing care.” This is armor you can actually wear.
Local Care That Doesn’t Feel Generic
Recovery isn’t one-size-fits-all—and neither is regional support.
If you’re in or around Plymouth County, you know the pace here: fast enough to keep up appearances, slow enough that people notice when you fall.
We tailor our recommendations to your life here. Not someone else’s idea of recovery.
If you’re outside the immediate area, we also support those looking for Intensive Outpatient Program IOP in Bristol County, MA.
FAQ: What If I’m Not Ready to Leave IOP?
How do I know if I’m ready to finish IOP?
If you’re asking this, it’s a good sign you’re taking your recovery seriously. Readiness isn’t about feeling “done”—it’s about having tools, support systems, and enough self-awareness to know what you still need.
Can I extend my time in IOP?
Absolutely. Many clients choose to extend, especially if new stressors are coming up (like work shifts, family changes, or triggering seasons). Talk to your clinician—we’ll make a plan that fits.
What if I leave IOP and relapse?
You can always come back. Waterside maintains an open-door policy. Relapse isn’t failure—it’s information. The real issue is staying disconnected, not “messing up.”
Do I have to do individual therapy after IOP?
It’s strongly encouraged. Group is powerful, but one-on-one support helps dig into personal patterns and fears that don’t always surface in a shared setting.
How does Waterside support alumni?
We offer alumni groups, therapy referrals, and optional step-down groups. You can also re-engage in higher levels of care without shame or judgment.
You’ve Built Something. Let’s Not Pretend You Didn’t.
The version of you that showed up to IOP? That version deserves credit. The version that’s scared to leave? That version deserves protection.
Don’t ghost your progress.
Don’t pretend you’re “fine” just because you can be.
Let’s build a next step that doesn’t just look strong—but actually feels supportive.
📞 Ready to take the next step?
Call 774-619-7750 or visit our Intensive Outpatient Program IOP page to learn more about IOP and aftercare options in Plymouth County, MA.